STARTING SOLIDS
Introducing foods to your baby is exciting but also can be overwhelming, but it doesn’t have to
be! While there are not a lot of rules for feeding babies, there are some guidelines that are
important, particularly in helping your child avoid food allergies, learn the necessary fine motor
skills to eat and drink as well as maintaining optimal nutrition.
When should you start?
Babies should be exclusively breastfed or formula fed until 4-6 months of age and most babies
are not ready to eat until closer to 6 months of age.
They are ready to start solid foods when they can:
● Maintain truncal support and sit up in the high chair
● Extinction of the extrusion reflex (the tongue pushing out anything that is put in the mouth)
● Interest in food
How to start solids?
There are three basic approaches to feeding babies: spoon-feeding, baby-led weaning or a
combination of both. Babies are fed differently all over the world and there is not a “right”
way. Either method, the goal would be to have your baby self feeding finger foods by 9
months.
● Spoon-feeding: this is the traditional method in which you start with pureed foods that
you give on a spoon. This is typically done for a few months and then finger foods are
offered around 8-9 months.
● Baby-led weaning: skipping pureed foods and going straight to letting babies feed
themselves with finger food.
While either method is okay, below are a few recommendations:
● Start with once a day feeds for the first few weeks as it lets their gastrointestinal
system get adjusted and helps avoid constipation. Then you can slowly increase to a
goal of 3 meals per day by 8-9 months.
● Start with a “whole” food. Historically, it was recommended to start with rice cereal.
This is no longer recommended as there is minimal nutritional value and can start with
any food such as avocado.
● It is important to remember that initially this is just practice and babies do not need this
nutrition and it is a time to explore new flavors and textures and to learn new fine
motor skills. With time, you can increase volume and textures.
● Do not give up if your baby seems to not like certain food. It can take 10-15 tries of a
food to develop a taste for it.
● Try new foods in the mornings so you can observe if your baby shows any signs of
allergic reaction.
● When starting finger foods, start with small bites of soft mashed foods like avocado,
banana, baked sweet potato or scrambled eggs. Food should be easily mashed with
fingers or a fork.
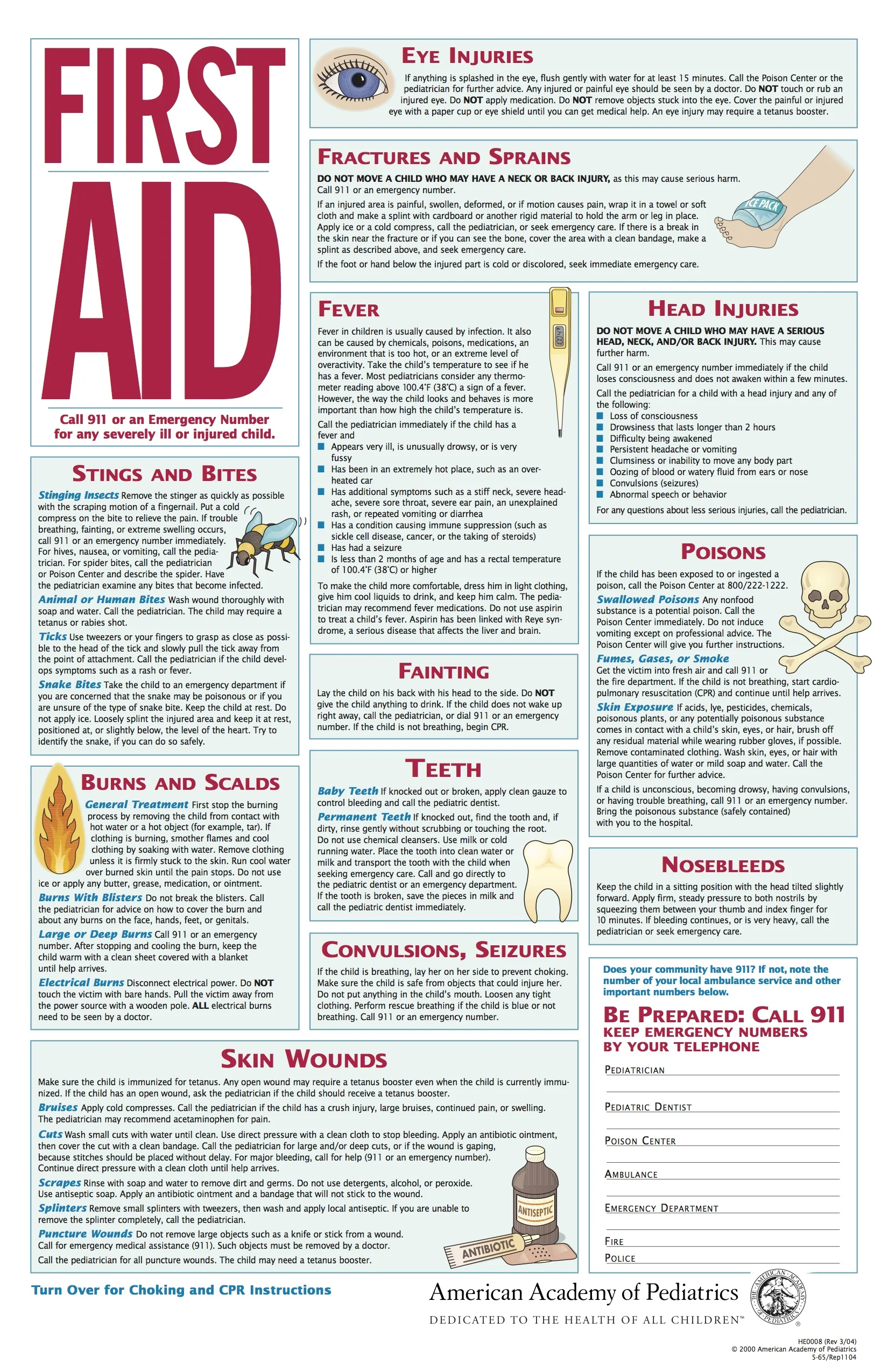
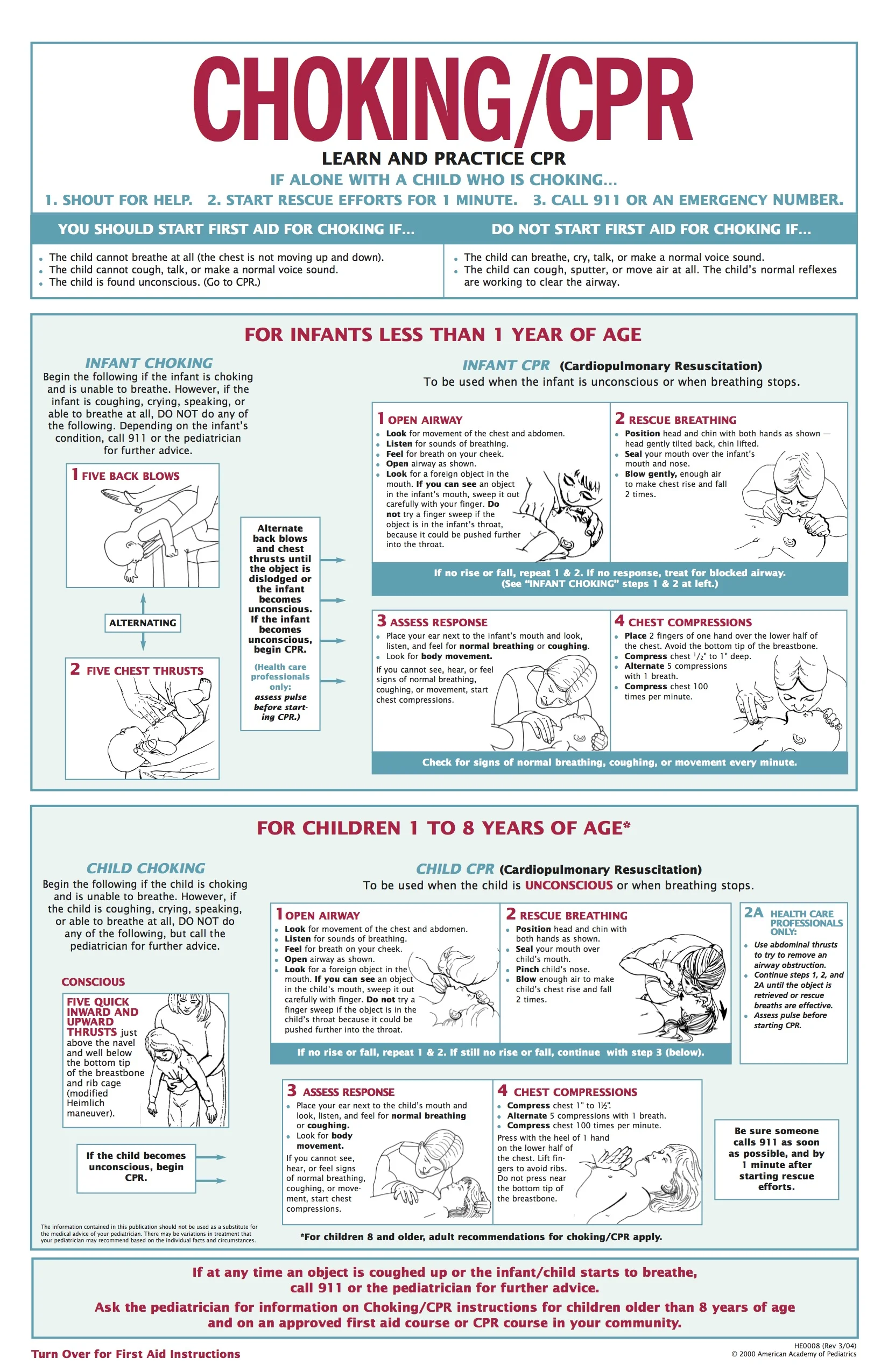
● We do recommend that all parents take a CPR class prior to starting solids.
● Never leave your child alone while eating solids.
What about water and how to give?
When you start food, you start water. Just like with solids, initially babies do not need a lot of
water and this is for exposure, but we recommend offering with all meals
● Offer water in something other than a bottle, such as a sippy cup, open cup or straw
cup. This is another opportunity to practice a new fine motor skill. We love the Ezpz
tiny cup!
What about allergic foods?
Food allergies are fairly common with approximately 10% of children having food allergies.
The good news is that there are some landmark clinical trials that early and sustained allergen
introduction helps to prevent allergies, particularly by 6 months. Children with eczema and a
family history of food allergies have a higher risk of developing food allergies, so it is
particularly important for these children to be introduced to food allergens early and often. If
there are risk factors, speak to your pediatrician before introducing solids.
The top three food allergens that make up 85% of allergies are:
● Dairy, peanuts and eggs.
● The top nine also include: tree nuts, sesame, wheat, soy, fish and shellfish.
So how do you introduce allergens?
If your baby is ready to eat, you can give the allergens directly. For example, you can mix a
small amount of peanut butter into oatmeal. There are other ways to introduce the allergens,
such as Ready Set Food. RSF is a supplement that is added to either a bottle or pureed food and it slowly introduces peanut, dairy and eggs. This is a safe way to introduce allergens
particularly if babies are at higher risk and not quite ready to eat solids.
While not necessary for non-allergic foods, it is important to:
● Give the allergic food three days in a row before introducing another allergen, if no
reaction, it is important to keep it in their diet regularly for the next 4-6 months.
Allergists recommend offering three times per week.
● Monitor for allergic reactions. Typical signs of an allergic reaction include hives, rash, swelling around the lips or vomiting. If there is any concern, then you should stop the food immediately and contact a physician. If you are concerned about difficulty
breathing or severe lethargy then call 911 for immediate help.
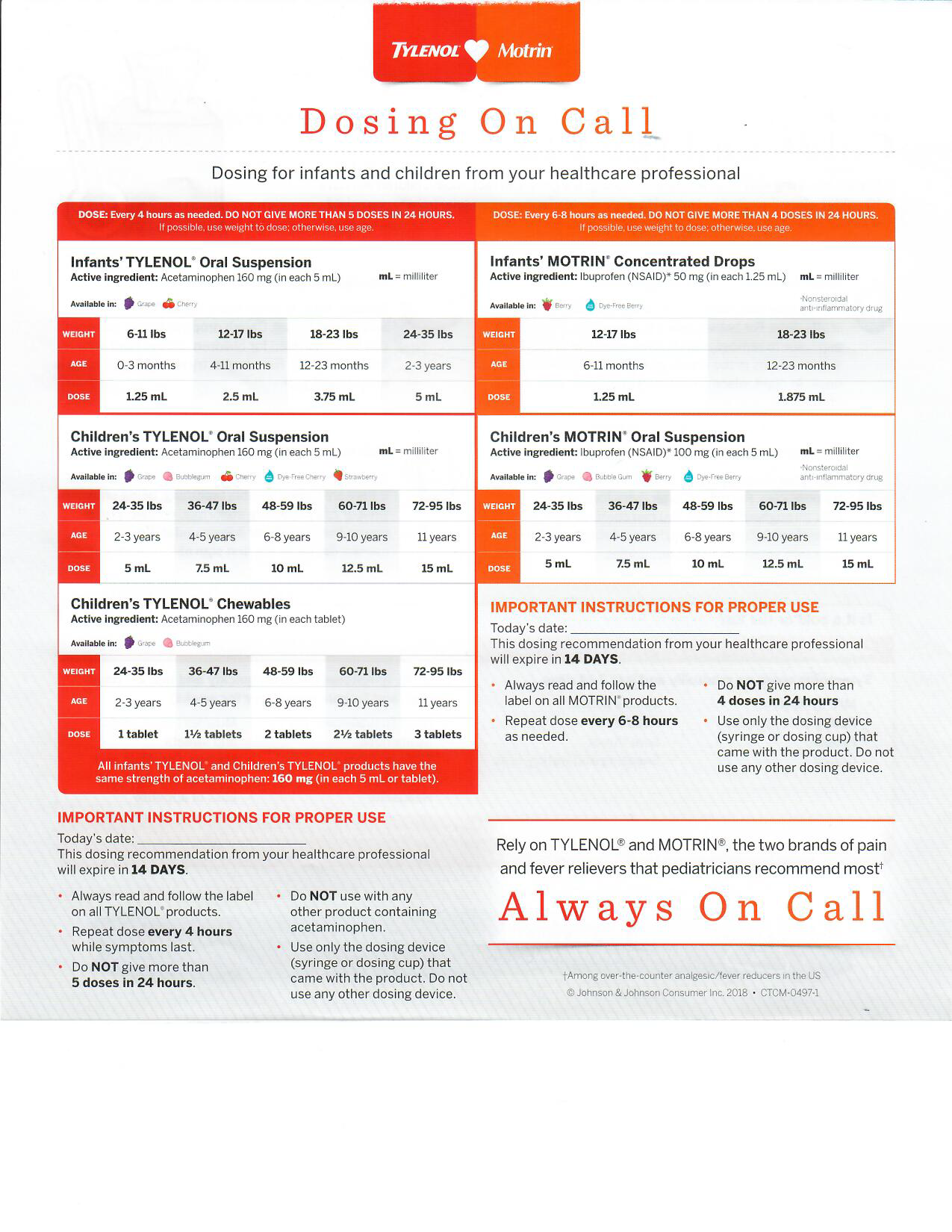
● It is a good idea to have liquid Benadryl on hand in case of a mild reaction. There is a
dosing chart on our website.
Other foods to introduce:
● Iron-rich foods: A baby has iron reserves from pregnancy until about 4-6 months of
age. After that age, breast fed babies need to eat foods rich in iron to prevent
iron-deficiency anemia. Formula has some iron, but babies still need more in their diet.
○ Iron supplementation may be recommended for some babies.
○ Iron rich foods include: Beans, meats, leafy greens, iron-fortified grains and
peas.
○ Cooking food in a cast-iron skillet can also increase the iron content of foods.
● Healthy fats: healthy fats are important as their brains continue to develop.
○ Healthy fats include: avocado, nut butters, salmon and whole-fat dairy products.
Foods to avoid:
● Until ONE year:
○ Honey: there is a risk of botulism with ingested honey
○ Whole milk: while it is okay to give dairy, such as cheese and yogurt, it is not
recommended to replace breast milk or formula with milk until then. Milk is
hard to digest and can increase risk of iron-deficiency anemia and does not have
all the nutrients that breast milk and formula have.
○ Sugars and processed foods are to be avoided as much as possible to ensure optimal nutrition.
● Choking hazards:
○ Avoid raw vegetables, nuts, seeds, popcorn, whole grapes (or other round
foods) hotdogs. These are all choking hazards. These foods can all be given, but need to be modified (i.e. grapes cut lengthwise).
Resources:
Baby led weaning:
https://solidstarts.com/
https://www.drorganicmommy.com/
https://www.yummytoddlerfood.com/first-foods-for-baby/
Instagram: Dawn Winkelmann, M.S.,SLP @msdawnslp
General feeding:
http://Healthychildren.org/
https://www.ellynsatterinstitute.org/
Allergy info:
https://readysetfood.com/
CPR info:
The Pump Station: www.pumpstation.com